When someone in the family suffers from dementia, the days are anything but easy. Time slips away from you as if the hours were marbles rolling across the floor. You are no longer in control of your time because it is entirely dedicated to them.
Personally, a perfect day might be one where there are no outbursts of anger. A day where there is no argument over taking a shower, or where you’re not hit while trying to put on their pajamas.
Many doctors offer lots of advice on how to handle these situations, but of course, every case is different.
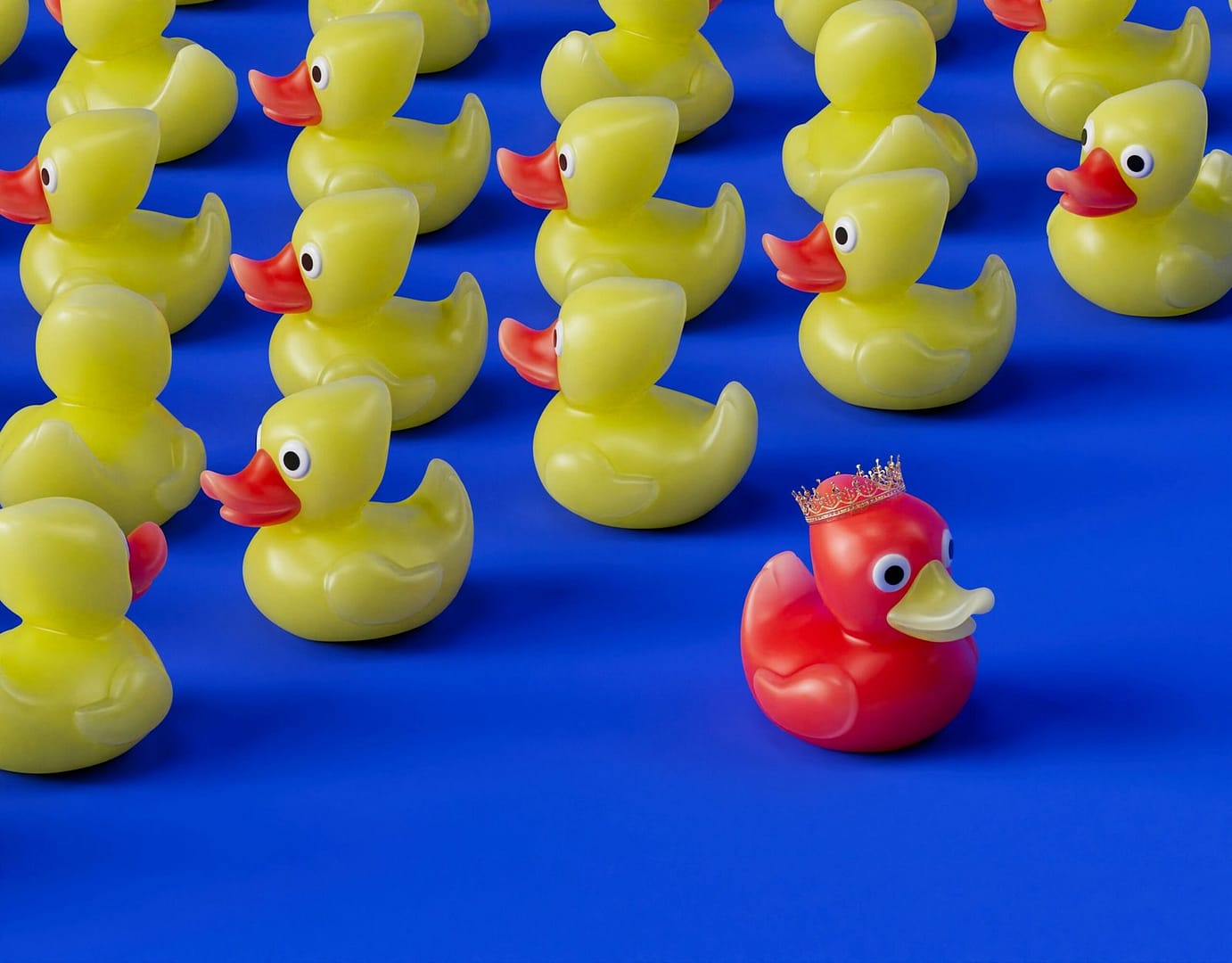
Someone once told me, “Play music while giving a shower, it will calm them down.” Or, “Buy some rubber ducks so your mom will see it as a game.”
The truth is, we don’t really know what’s going through their heads. We can’t just categorize them as children who are being fussy or as little animals frightened by everything. My mom is afraid of water, plain and simple. No rubber ducks or music will make a difference.
Dementia and Phobias
Indeed, just reading clinical case studies is enough to correlate Dementia and Phobias.
Aquaphobia, defined as “an abnormal and persistent fear of water,” can be connected to heart disease, gastrointestinal diseases, respiratory diseases, arthritic conditions, migraines, and thyroid disorders. People who suffer from a fear of water feel anxious even though they recognize that water may not pose an immediate threat. Typically, they avoid activities such as swimming and boating. For example, at home, they might fear the water in the shower and even avoid bathing altogether. For others, the experience of being lifted can be distressing. Some may experience panic attacks, which can be quite debilitating and embarrassing.
Some people may react with heightened alertness during bath time due to embarrassment, especially if they still have feelings about privacy and appropriate behavior. Therefore, bathing can often be traumatic for elderly adults, who feel embarrassed to need help during such a personal moment in their day.
Others, who have already fallen on a slippery surface, may associate water with painful injuries.
Doctors often say it’s important to approach people slowly. For instance, by practicing deep breathing and relaxation exercises, encouraging the person, celebrating small successes, and accepting that overcoming fear is a process that takes time and patience. But how can you apply this when you’re dealing with someone with dementia or Alzheimer’s?
At the Mayo Clinic, an international institute I consulted for neurological information for my mother, they suggest that cognitive-behavioral therapy might work better than medication.
But how does it work if the patient is neither capable of attending a psychotherapy session nor able to understand you 100% of the time?
According to this study on “Cognitive Behavioral Therapy for Patients with Dementia,”
the study shows how cognitive-behavioral therapy can be adapted for patients with dementia. The question is, why aren’t we doing more for our elderly? Why is everything so difficult, and why do we have to go to the USA to find news and resources?

Leave a Reply